Accelerate medical claims with AI-powered insights—watch MedReview in action.
THE CHALLENGE
Medical documents are lengthy, complex, and highly specialized. Manual review is time-consuming, error-prone, and unsustainable under the pressure of rising claims volumes. Delays lead to customer dissatisfaction and increased operational costs.
OUR SOLUTION
By harnessing 360 MedReview, legal and claims professionals gain the ability to instantly parse medical data, identify key points, and summarize findings. This accelerates claim settlements and ensures consistent regulatory compliance.
360 MedReview standardizes medical summarization across diverse records—clinic notes, ER reports, imaging, billing—so clinical and legal teams work from the same facts. It extracts diagnoses, treatments, timelines, providers, and billed vs. allowed amounts, then builds a readable chronology with citations to the original pages. Confidence flags highlight what needs human confirmation; everything else flows into your templates and systems. Configure the data model to your venue and practice patterns, keep an audit trail for every entry, and export clean packets for counsel, adjusters, or oversight. The result is faster reviews, fewer misses, and consistent outputs your teams can trust.
Key Benefits
Unlock measurable impact across speed, accuracy, and cost with AI-powered medical document automation.

Time Efficiency
Dramatically reduce review times for medical documents, enabling teams to handle a higher volume of cases simultaneously.
.png)
.png)
Cost Savings
With faster turnaround and fewer errors, organizations can minimize operational overhead and legal exposure
.png)
Improved Accuracy
Advanced AI reduces human error, ensuring consistent and reliable data extraction—leading to more confident claim decisions.
.png)
Faster Claim Settlements
.png)
Quicker document processing directly translates into faster approvals or settlements, boosting policyholder satisfaction.
Competitive Advantage
Offering rapid, tech-enabled medical claims review sets you apart, attracting more clients and reinforcing your reputation for innovation.
See MedReview in Action
This short demo shows how MedReview accelerates medical claims by using advanced OCR, AI, and GPT to instantly extract, analyze, and summarize critical medical data.
Key Features
Built for speed, accuracy, and compliance—every feature is designed to simplify and secure medical claims review.
OCR
Technology
Accurately extracts text from scanned or faxed documents, drastically minimizing the manual workload.
AI, LLM, and
GPT Integration
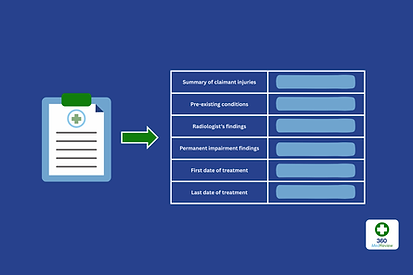
Advanced machine learning models interpret clinical information, identify relevant injuries or diagnoses, and generate succinct summaries.
Customizable Summarization Templates
Tailor the system to capture exactly what your claims or legal team needs—like treatment dates, objective/subjective findings, or procedure codes.
Real-time Data Processing
Summaries are generated instantaneously, enabling quick decisions and timely follow-ups.
Secure & Compliant
Built on trusted enterprise-grade infrastructure, 360 MedReview supports secure data handling and compliance across a wide range of regulatory environments.

.png)